Healthcare is a glaring concern due to high costs and various challenges it poses. However, the issues extend beyond that, including frequent false positives in diagnoses and mistakes in surgery, which contribute to uncertainty in outcomes. With the rise of large language models (LLMs), one might wonder how they can improve healthcare. Healthcare, as of today, is on the path to becoming not only more affordable but also more reliable by virtue of LLMs. This article highlights the state of AI advancements in healthcare, along with the latest breakthroughs that are addressing problems at an unprecedented scale and precision.
Table of contents
Current Status of Healthcare
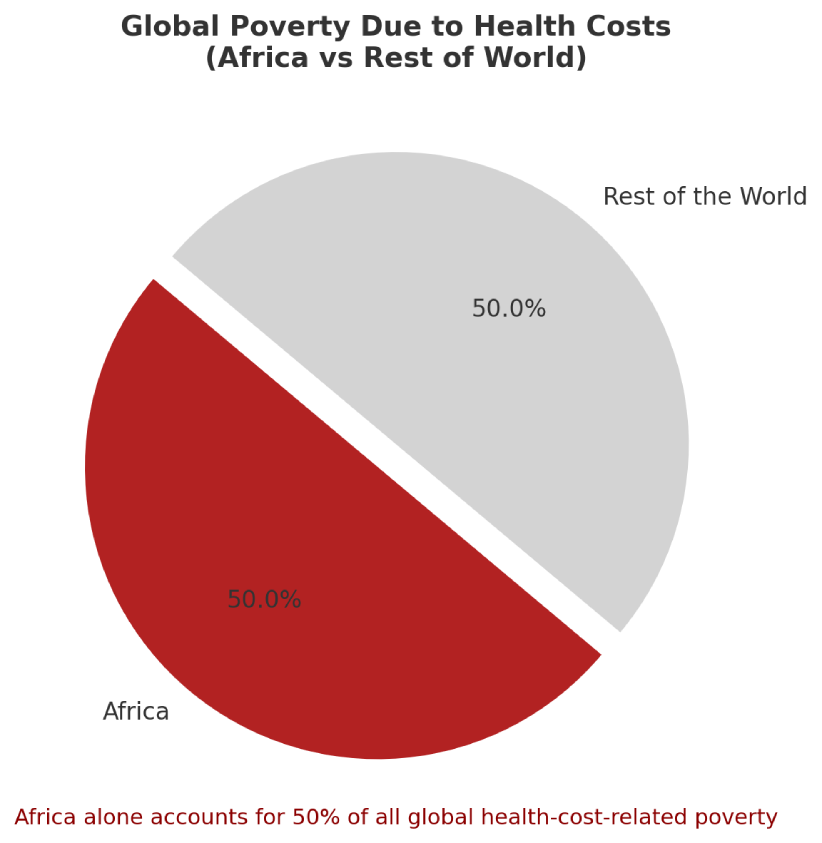
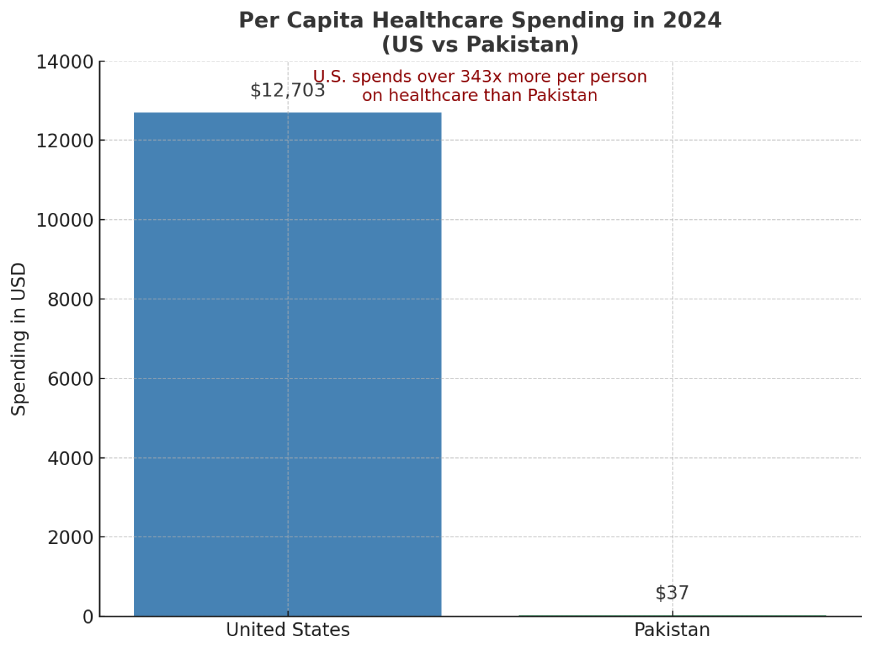
Across the world, healthcare costs are high and particularly uneven. Good healthcare is an opulence in some countries due to cost and equity, and a problem in others via a lack of quality and access. About half the world lacks essential health coverage, and over a billion people face severe financial hardship from medical bills. Spending per person varies dramatically! A survey projects US$12,703 per capita in the US vs just $37 in Pakistan by 2024, reflecting vast inequities in medical expenditure. Out‐of‐pocket payments remain a heavy burden in poorer regions. In Africa, the WHO estimates that over 150 million people were pushed into poverty by health costs. Also, half of all global health‐cost impoverishment occurs in Africa. These figures underscore that a basic amenity like healthcare at some places might actually be a luxury.
Setting the Stage for AI
Unlike technical domains where AI came in and found a home, its journey in healthcare was a long and elaborate one. The domain isn’t ripe for its total inclusion, but the stage has been set following certain developments.
Telemedicine and Digital Transformation
Telemedicine consultations and remote monitoring have become common since COVID-19 and remain far above pre-2020 levels. By mid-2021, telemedicine stabilized at about 13–17% of all outpatient visits. This persistent use reflects patient and provider demand. A Deloitte survey found ~80% of consumers intend to have another virtual visit post-pandemic. Analysts estimate that up to 20% of U.S. healthcare spending (~$250 billion) could potentially be delivered virtually if broadly adopted. In other words, remote care could shift vast volumes of care online, potentially cutting costs without sacrificing access.
The Rise of AI in Healthcare
Artificial Intelligence has gradually become a foundational part of modern healthcare. From assisting in medical imaging to automating diagnosis, AI has proven valuable for reducing human error and increasing efficiency. It also allowed access to services at places where it wasn’t available before. While the early AI tools focused on narrow tasks, such as flagging anomalies in X-rays for diagnostics or predicting hospital re-admissions for insurance. But recent advancements have enabled AI systems to reason and interpret complex medical data. At the heart of this evolution are large language models, which present a new frontier in healthcare. The technology provides models that go beyond task automation, providing tools that can analyze, interpret, and even simulate real-life scenarios.
Latest Developments in Medical LLMs
The latest healthcare developments by Microsoft and Google, namely MedGemma (by Google) and MAI-DxO (by Microsoft), are deeply rooted in LLMs. They leverage LLMs for clinical reasoning, medical report generation, and augment clinical practitioners in their decision-making.
MedGemma
Google has released two new open models for healthcare AI: MedGemma 27B Multimodal and MedSigLIP. This effort was towards expanding their MedGemma collection under the Health AI Developer Foundations (HAI-DEF) initiative.
- MedGemma 27B Multimodal can handle both text and images, making it useful for generating medical reports. It scores 87.7% on the MedQA benchmark, rivaling larger models at a fraction of the cost.
- MedSigLIP is a 400M-parameter image-text encoder trained on medical images (like chest X-rays and pathology slides). It’s ideal for classification, image search, and zero-shot tasks, and still performs well on general images too.
Both models are open-source, run on a single GPU, and can be fine-tuned for specific use cases. Smaller variants like MedGemma 4B and MedSigLIP can even run on mobile devices.
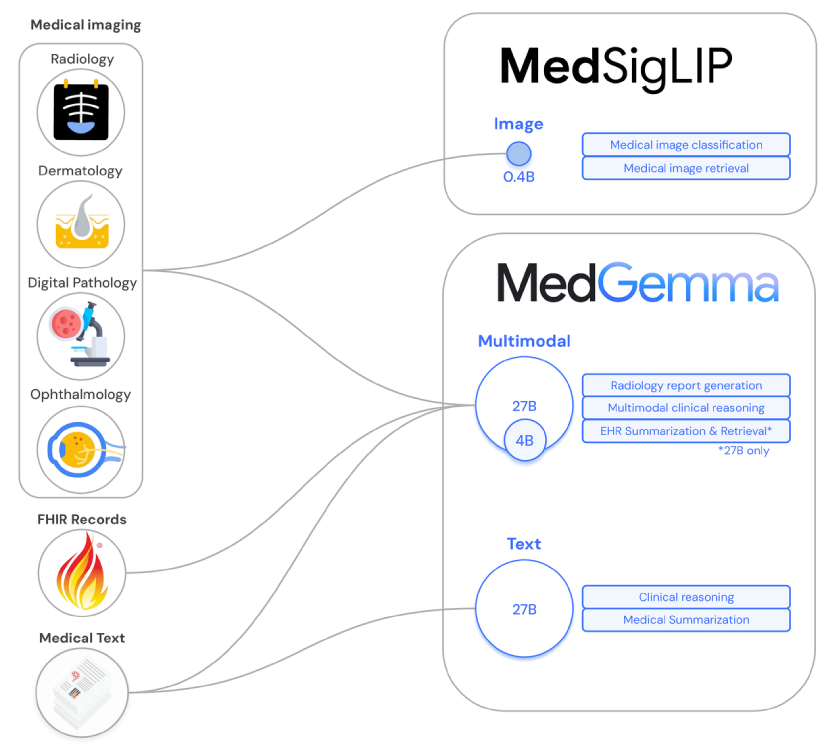
Developers are already using these LLMs for real-world tasks: X-ray triage, clinical note summarization, and even multilingual medical Q&A. Google also provides sample code, deployment guides, and demos on Hugging Face and Vertex AI.
MAI-DxO
Microsoft’s AI Diagnostic Orchestrator (MAI-DxO) is a new system designed to tackle medicine’s toughest diagnostic challenges. The model outperforms physicians in both accuracy and cost-efficiency. Tested on 304 real clinical cases from the New England Journal of Medicine, MAI-DxO achieved up to 85.5% diagnostic accuracy, over 4x higher than a group of experienced doctors (average 20%). It works by simulating how clinicians gather and evaluate information step-by-step, instead of relying on multiple-choice answers. Each diagnostic action is tracked with virtual cost, showing MAI-DxO is smarter and more efficient than traditional methods.
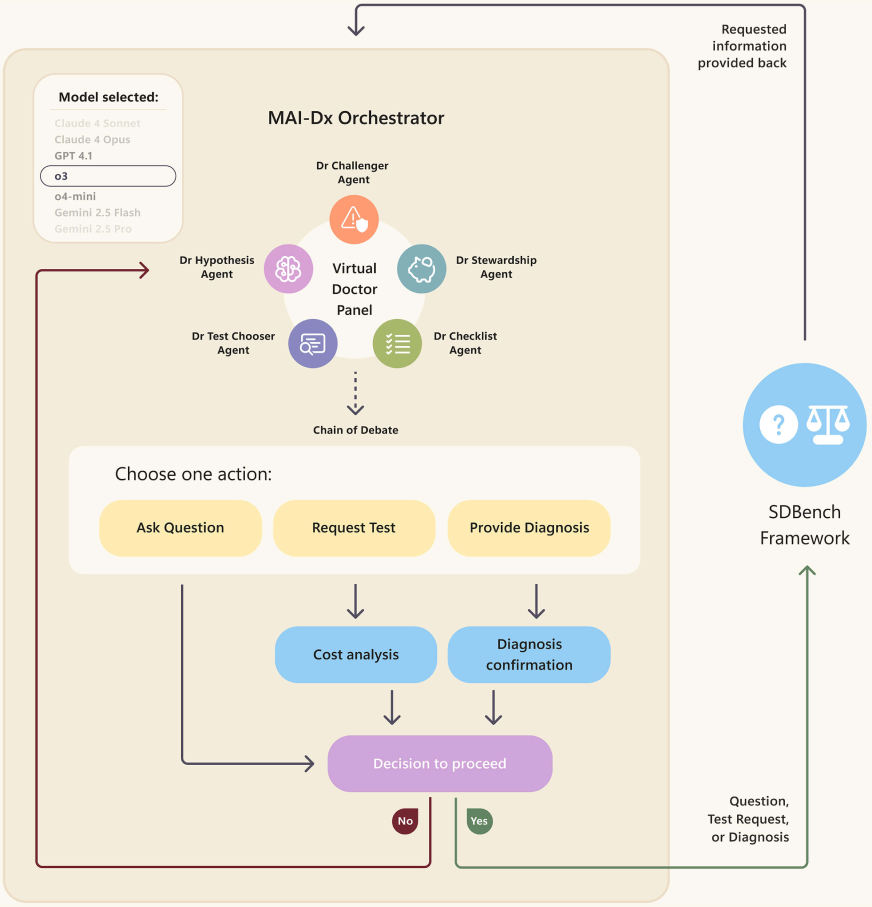
This work builds on Microsoft’s broader health AI efforts, including Dragon Copilot for clinicians and RAD-DINO for radiology. A key innovation is the orchestrator’s ability to coordinate multiple LLMs, acting like a panel of virtual physicians that collaborate to reach a diagnosis. Microsoft’s research team sees this as a major step toward responsible, trustworthy AI in healthcare, especially for complex cases.
Impact due to Artificial Intelligence Adoption
Artificial intelligence, including LLMs, is offering improvements in the efficiency of several workflows. A recent estimate indicates that broader AI adoption could reduce U.S. health spending by 5–10%, roughly $200–360 billion annually. AI tools can automate tasks such as clinical documentation, diagnostics, and administrative assistance. However, experts highlight that these benefits depend on appropriate infrastructure and costs. In practice, health systems need to weigh customized AI solutions against tools, in which the options range from developing new models to using external services. The decision depends on system requirements and cost considerations. Overall, while LLMs can lower healthcare costs by increasing efficiency, they require significant initial investments in the technology.
Mixed Signals and Remaining Challenges
Overall, affordability is improving unevenly in spite of these trends. Here are some of the challenges in health affordability and healthcare systems:
- Uneven improvement: While there are positive trends, the improvements in healthcare affordability are not consistent across countries or populations (apparent from the African example).
- Promising tools exist, but costs are still rising: Government policy changes and solutions like telehealth and AI show promise, but many areas are still experiencing rising healthcare costs.
- Catastrophic health expenses remain common: According to World Bank experts, many people still face catastrophic health expenditures, pushing them into poverty due to medical costs.
- Health coverage progress has stalled since 2015: Global advances in health coverage have largely plateaued, with little progress made in recent years.
- Most countries lack full protection: Per the WHO, out-of-pocket expenses remain high in many regions, and only 30% of countries have improved both health coverage and financial protection simultaneously.
Conclusion
Technology and policy are moving toward more affordable care through LLMs and AI, but a gap remains. Billions still lack access to affordable services. Achieving affordable healthcare worldwide will require digital adoption, smart financing, and continuous innovation – efforts that some high-income countries are advancing quickly, but that poorer countries are yet to instigate. With the release of these colossal healthcare LLMs, the gap has been narrowing between these disparate regions. The outlook is hopeful but incomplete: we have tools to lower healthcare costs, yet the global implementation and acceptance of such tools is far from home.
Frequently Asked Questions
A. The answer is mixed. Healthcare affordability is improving unevenly globally. AI, telemedicine, and generics offer cost savings potential, but rising costs and billions facing financial hardship mean implementation is incomplete.
A. LLMs and AI improve diagnostics, automate admin tasks, and enhance clinical efficiency, potentially saving billions. Benefits rely on infrastructure and trained staff.
A. Telemedicine use rose post-COVID, stabilizing at 13-17% of visits with 80% patient reuse intent. It can cut costs and shift $250B of US care virtually.
A. Generics and pricing policies cut costs. The generic drug market will grow 50% by 2028. US Medicare saved $6B on drug prices in 2023 through negotiation.
A. Challenges include global inequities, catastrophic costs, stalled coverage progress, and the need for infrastructure. Only 30% of countries improve coverage and financial protection simultaneously.